What Is a Craniotomy? Types, Risks, and Recovery
A craniotomy is one of the most critical and complex procedures in the field of neurosurgery. It is a surgical operation where a piece of the skull—called a bone flap—is temporarily removed to allow a neurosurgeon access to the brain. Once the underlying issue is treated, the bone flap is typically replaced and secured with small titanium plates and screws.
Whether you are preparing for a scheduled procedure or seeking information following an emergency, understanding the “why” and “how” of a craniotomy is essential. This guide provides a comprehensive look at the different types of craniotomies, the risks involved, and the detailed roadmap to recovery.
1. Why is a Craniotomy Performed?
A craniotomy is not a treatment in itself; rather, it is the surgical “doorway” that allows doctors to treat various neurological conditions. Common reasons for performing a craniotomy include:
- Brain Tumors: To remove or debulk a tumor (resection) or to take a tissue sample (biopsy).
- Aneurysms: To “clip” a weakened blood vessel to prevent it from rupturing.
- Traumatic Brain Injury (TBI): To remove blood clots (hematomas) or to stop internal bleeding after a head injury.
- Epilepsy: To remove small areas of the brain where seizures originate.
- Brain Abscesses: To drain an infection within the brain tissue.
- Microvascular Decompression: To relieve pressure on a nerve caused by a blood vessel (often used for trigeminal neuralgia).
2. The Difference: Craniotomy vs. Craniectomy
It is common to confuse these two terms, but the difference is vital:
- Craniotomy: The bone flap is replaced at the end of the surgery.
- Craniectomy: The bone flap is not replaced immediately. This is usually done to allow the brain to swell without being crushed against the skull. The bone is typically replaced months later in a procedure called a cranioplasty.
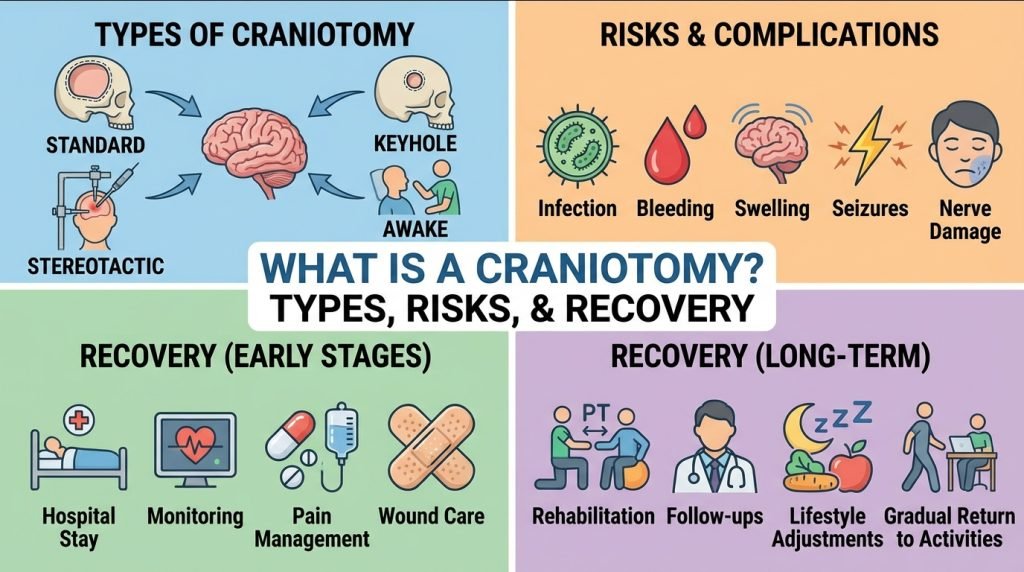
3. Specialized Types of Craniotomy
Advancements in surgical technology have allowed neurosurgeons to tailor the procedure to the specific needs of the patient.
Awake Craniotomy
This is often used for tumors located near “eloquent” areas of the brain—parts that control speech, movement, or vision. The patient is woken up during the middle of the surgery to perform tasks (like talking or moving fingers) to ensure the surgeon does not damage critical pathways.
Keyhole Craniotomy (Minimally Invasive)
Instead of a large incision, the surgeon uses a tiny opening (often behind the ear or in the eyebrow) to reach the target area using an endoscope. This leads to faster recovery and less scarring.
Stereotactic Craniotomy
This utilizes GPS-like computer navigation. Before surgery, an MRI or CT scan is performed to create a 3D map of the brain. The surgeon uses this map during the procedure to find the most direct and safest route to the tumor or lesion.
Extended Bifrontal Craniotomy
This involves removing the bone that forms the forehead and the roof of the eye sockets. It is typically used for complex tumors located at the very base of the brain (skull base).
4. Understanding the Risks of Brain Surgery
While craniotomies are performed every day by highly skilled teams, all brain surgeries carry inherent risks.
- Infection: At the incision site or within the brain (meningitis).
- Hemorrhage: Bleeding in the brain during or after the procedure.
- Seizures: The brain is a sensitive electrical organ; manipulating it can trigger post-operative seizures.
- Neurological Deficits: Depending on the area of the brain being treated, there is a risk of temporary or permanent changes in speech, memory, vision, or muscle strength.
- Cerebrospinal Fluid (CSF) Leak: Fluid can leak through the surgical opening in the dura (the brain’s protective covering).
- Brain Swelling (Edema): The brain’s natural response to surgery is to swell, which must be carefully managed with medications.
5. The Recovery Timeline: What to Expect
Recovery from a craniotomy is a gradual process that happens in phases. Every patient’s journey is unique depending on the reason for the surgery.
Phase 1: The Hospital (3–7 Days)
- ICU Stay: You will likely spend the first 24–48 hours in the Neuro-ICU for constant monitoring of your neurological status.
- Monitoring: Nurses will frequently ask you your name, where you are, and to squeeze their hands to check brain function.
- Pain Management: Expect a headache and some soreness at the incision site. This is managed with IV or oral medications.
Phase 2: Early Recovery at Home (Weeks 1–4)
- Activity: You will feel very tired. Short walks around the house are encouraged, but heavy lifting and strenuous exercise are strictly prohibited.
- Incision Care: You must keep the incision clean and dry. Most surgeons advise against washing your hair for the first week.
- Driving: You cannot drive until your surgeon clears you, especially if you are taking anti-seizure medications.
Phase 3: The “New Normal” (Months 1–6)
- Bone Healing: It takes about 6 to 12 months for the bone flap to fully fuse back with the rest of the skull.
- Return to Work: Depending on the nature of your job, many patients return to work in 6 to 12 weeks.
- Rehabilitation: Some patients require physical, occupational, or speech therapy to regain lost functions.
6. Tips for a Successful Recovery
- Follow the “BLT” Rule: No Bending, No Lifting (over 5 lbs), and No Twisting for the first several weeks.
- Monitor Your Mood: It is common to experience “post-craniotomy blues” or anxiety. Your brain is healing chemically as well as physically.
- Stay Hydrated: Dehydration can worsen post-operative headaches.
- Listen to Your Brain: If you feel a “pressure headache” or extreme fatigue, it is a sign you are overexerting yourself.