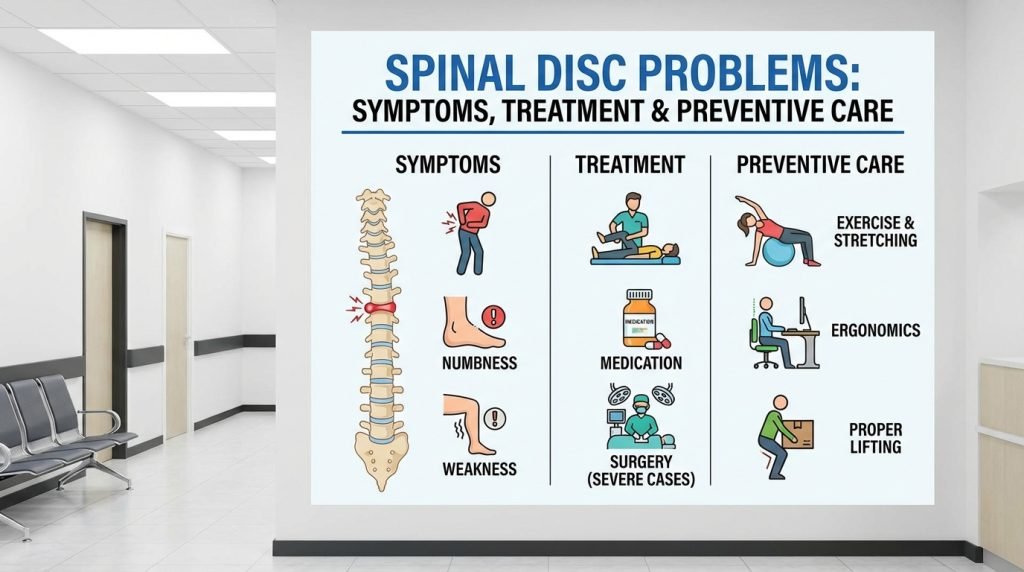
Spinal Disc Problems: Symptoms, Treatment & Preventive Care
Back pain is one of the most common reasons people seek medical attention or miss work worldwide. At the heart of many of these issues are the intervertebral discs—the specialized cushions located between the bones of your spine (vertebrae). When these discs become damaged, dehydrated, or displaced, the resulting pain can be debilitating.
Understanding the nuances of spinal disc problems, from a minor bulge to a severe herniation, is essential for choosing the right treatment path. This guide covers everything you need to know about symptoms, modern treatments, and how to keep your spine healthy for years to come.
1. The Anatomy of a Spinal Disc: Your Body’s Shock Absorbers
To understand what goes wrong, you must first understand how a healthy disc works. Your spine consists of 33 vertebrae, and between each one (except the first two in the neck) sits a spinal disc.
Each disc has two main parts:
- Annulus Fibrosus: The tough, flexible outer ring made of collagen fibers.
- Nucleus Pulposus: The soft, jelly-like center that provides cushioning and flexibility.
Think of the disc like a jelly donut. When the “donut” is compressed or the outer ring tears, the “jelly” can leak or bulge out, irritating nearby nerves.
2. Common Types of Spinal Disc Problems
Not all spinal pain is the same. Disc issues generally fall into three main categories:
Herniated Disc (Slipped Disc)
A herniated disc occurs when the nucleus pulposus pushes through a tear in the annulus fibrosus. This “leaking” jelly often chemically irritates the spinal nerves or physically compresses them, leading to sharp, radiating pain.
Bulging Disc
Unlike a herniation, a bulging disc involves the outer layer remaining intact, but the entire disc “spills” over the edge of the vertebrae. It is often a result of age-related wear and tear and may not always cause pain unless it touches a nerve.
Degenerative Disc Disease (DDD)
This is not actually a “disease” but a condition where the discs naturally lose water content and elasticity as we age. This causes the discs to thin, reducing the space between vertebrae and potentially leading to bone spurs or spinal stenosis.
3. Recognizing the Symptoms: Is It Just a Sore Muscle?
Symptoms of disc problems vary depending on where the affected disc is located—the cervical spine (neck) or the lumbar spine (lower back).
Lumbar Disc Symptoms (Lower Back)
- Sciatica: A sharp, shooting pain that travels from the buttock down the back of the leg.
- Numbness or Tingling: A “pins and needles” sensation in the feet or toes.
- Muscle Weakness: Difficulty lifting the front of the foot (foot drop) or weakness when standing up from a chair.
Cervical Disc Symptoms (Neck)
- Radiating Arm Pain: Pain that travels down the shoulder and into the arm or hand.
- Grip Weakness: Difficulty holding objects or performing fine motor tasks like buttoning a shirt.
- Stiff Neck: Limited range of motion and dull aches between the shoulder blades.
Red Flag Symptoms: When to Seek Emergency Care
In rare cases, a disc herniation can cause Cauda Equina Syndrome. Seek immediate medical attention if you experience:
- Loss of bladder or bowel control.
- “Saddle anesthesia” (numbness in the inner thighs or groin).
- Sudden, severe weakness in both legs.
4. How Spinal Disc Problems are Diagnosed
A clear diagnosis is the foundation of recovery. A specialist will typically use a combination of the following:
- Physical Exam: Checking your reflexes, muscle strength, and ability to feel light touch. The “Straight Leg Raise” test is a common way to check for lumbar disc issues.
- MRI (Magnetic Resonance Imaging): The most effective tool for seeing soft tissues like discs and nerves.
- CT Scan: Useful for seeing the bony structures of the spine and how they might be encroaching on the spinal canal.
- Electromyography (EMG): Tests the electrical activity of your nerves to determine exactly which nerve root is being compressed.
5. Modern Treatment Options: From Conservative to Surgical
The good news is that over 80% of patients with disc problems recover without surgery within six to eight weeks.
Non-Surgical Treatments
- Physical Therapy (PT): A tailored exercise program to strengthen the “core” muscles that support the spine.
- Epidural Steroid Injections (ESI): Injecting anti-inflammatory medication directly near the irritated nerve to reduce swelling and pain.
- Medications: NSAIDs (like ibuprofen) for inflammation, muscle relaxants for spasms, or nerve pain medications (like gabapentin).
- Spinal Decompression Therapy: Using a traction table to gently stretch the spine, creating negative pressure within the disc to help a bulge “retract.”
Surgical Treatments
If conservative treatments fail after several months, or if neurological deficits (like weakness) worsen, surgery may be necessary:
- Microdiscectomy: A minimally invasive procedure to remove the portion of the disc that is pressing on the nerve.
- Laminectomy: Removing a small piece of the vertebra (the lamina) to create more space for the spinal cord.
- Artificial Disc Replacement: Replacing the damaged disc with a mechanical one, preserving the spine’s mobility.
- Spinal Fusion: Joining two vertebrae together to eliminate painful movement between them.
6. Preventive Care: How to Protect Your Spine
Prevention is always better than a cure. You can significantly reduce your risk of disc injury by following these lifestyle habits:
Master Your Posture
Whether sitting at a desk or standing, keep your ears aligned over your shoulders and your shoulders over your hips. Avoid “tech neck” by bringing your phone up to eye level instead of looking down.
Use Proper Lifting Techniques
Never bend at the waist to pick up heavy objects. Instead, bend at the knees and hips (the “hip hinge”) and keep the object close to your body.
Core Strength is Key
Your abdominal and back muscles act as a natural “brace” for your spine. Exercises like planks, bird-dogs, and dead-bugs are excellent for building spinal stability.
Maintain a Healthy Weight
Excess body weight, especially around the abdomen, pulls the pelvis forward and puts extra strain on the lumbar discs.
Stay Hydrated and Stop Smoking
Discs need water to stay plump and functional. Furthermore, smoking restricts blood flow to the spinal discs, causing them to degenerate much faster than they would naturally.