Common Causes of Persistent Headaches & When to See a Neurosurgeon
Almost everyone experiences a headache at some point, but when a “simple headache” becomes a persistent, daily, or worsening condition, it transitions from a nuisance to a medical concern. Persistent headaches—often defined as occurring 15 or more days a month—can significantly diminish your quality of life and, in some cases, signal a serious underlying neurological issue.
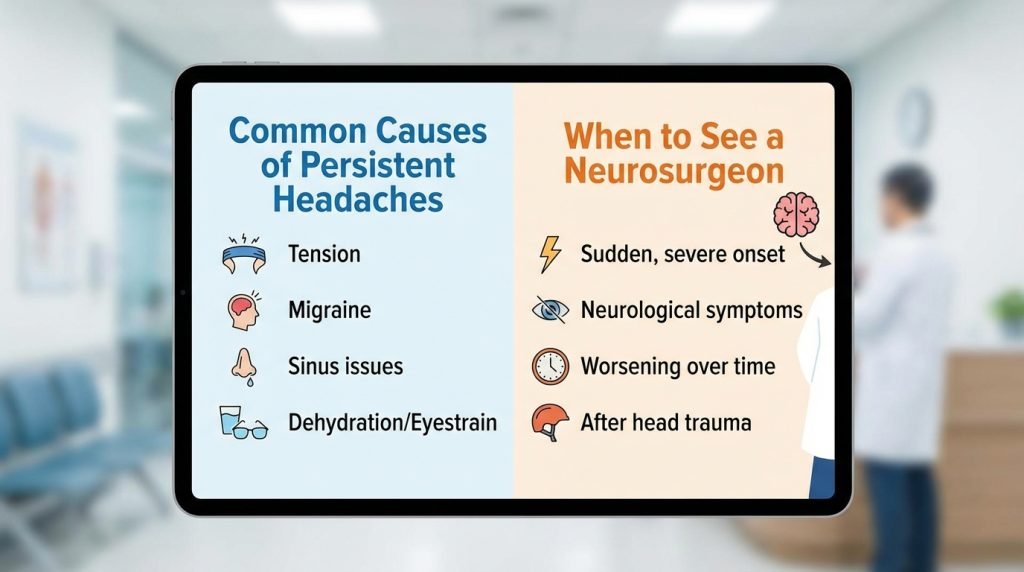
Understanding the difference between a primary headache disorder (like a migraine) and a secondary headache (caused by an underlying structural issue) is critical. This guide explores the common causes of chronic head pain and identifies the “red flags” that indicate it is time to consult a neurosurgeon.
1. Defining Persistent Headaches: Primary vs. Secondary
To understand the cause, we must first categorize the headache.
Primary Headaches
These are standalone conditions caused by overactivity of pain-sensitive structures in the head. They are not symptoms of another disease.
- Tension-Type Headaches: The most common variety, often feeling like a tight band around the head.
- Migraines: Intense, pulsing pain often accompanied by nausea and sensitivity to light/sound.
- Cluster Headaches: Severe, piercing pain usually localized around one eye.
Secondary Headaches
These are symptoms of another condition that stimulates the pain-sensitive nerves of the head. This is where neurosurgical intervention often becomes relevant. Causes include:
- Brain tumors or cysts.
- Aneurysms or vascular malformations.
- Cerebrospinal fluid (CSF) leaks or pressure imbalances.
- Traumatic brain injuries (TBI).
2. Common Causes of Persistent Headaches
Chronic Migraine
Chronic migraine is diagnosed when a person has a headache on 15 or more days a month, with at least 8 of those days having migraine features. While often managed by neurologists, chronic migraines that resist all medication sometimes require a neurosurgeon to evaluate for nerve decompression or underlying structural triggers.
Occipital Neuralgia
This condition involves the inflammation or injury of the occipital nerves, which run from the top of the spinal cord up through the scalp. It causes piercing, throbbing, or electric-shock-like pain in the upper neck and back of the head.
Cervicogenic Headaches
These are “referred pain” headaches caused by issues in the cervical spine (the neck). Herniated discs, osteoarthritis, or spinal stenosis in the neck can compress nerves, leading to persistent headaches that seem to radiate from the base of the skull.
Medication Overuse Headaches (Rebound Headaches)
Ironically, the frequent use of pain relievers (NSAIDs, triptans, or opioids) can cause the brain to become hypersensitive, leading to a cycle of “rebound” headaches as the medication wears off.
3. When a Headache Signals a Surgical Issue
While most headaches are managed medically, certain symptoms suggest that the brain’s physical structure is compromised. This is when the expertise of a neurosurgeon is required.
Intracranial Hypertension (High Pressure)
Conditions like Idiopathic Intracranial Hypertension (IIH) occur when there is too much cerebrospinal fluid in the skull. This creates pressure that mimics a brain tumor, causing persistent headaches and potential vision loss. Neurosurgeons may treat this by installing a shunt to drain excess fluid.
Brain Tumors and Cysts
A tumor does not always cause “sharp” pain. Instead, it often creates a dull, persistent ache that is worse in the morning or worsens with coughing, sneezing, or bending over. As the tumor grows, it increases intracranial pressure, necessitating surgical evaluation.
Chiari Malformation
This is a structural defect where brain tissue (the cerebellum) extends into the spinal canal. A hallmark symptom is a headache that begins at the back of the head and is triggered by straining, laughing, or physical exertion. Neurosurgeons perform decompression surgery to create more space for the brain and restore normal fluid flow.
Brain Aneurysms and Arteriovenous Malformations (AVMs)
A “thunderclap” headache—a sudden, excruciating pain that reaches peak intensity within seconds—is a medical emergency. It often indicates a ruptured aneurysm. However, unruptured aneurysms or AVMs can also cause persistent, localized pressure that requires surgical “clipping” or “coiling.”
4. The “Red Flags”: When to See a Neurosurgeon
If you experience any of the following, you should request a referral to a neurosurgeon for a specialized evaluation:
- The “Thunderclap” Onset: A sudden, severe headache unlike anything you’ve felt before.
- Neurological Deficits: Numbness, weakness, loss of balance, or difficulty speaking alongside the headache.
- Vision Changes: Blurred vision, double vision, or a “halo” effect.
- Positional Pain: Headaches that significantly change in intensity when you lie down vs. stand up (often a sign of CSF pressure issues).
- Seizures: New-onset seizures in an adult with persistent headaches are a major red flag for a structural lesion.
- Failed Medical Management: If you have seen a primary care doctor or neurologist and your headaches remain refractive to all medications, a neurosurgeon can investigate structural causes that may have been overlooked.
5. Diagnostic Steps in Neurosurgery
A neurosurgeon uses advanced diagnostics to look “under the hood” of your headache.
- MRI with Contrast: The gold standard for identifying tumors, inflammation, and structural defects like Chiari Malformation.
- CT Angiography (CTA): Focuses on the blood vessels in the brain to rule out aneurysms or vascular issues.
- Lumbar Puncture (Spinal Tap): Measures the pressure of the cerebrospinal fluid to diagnose high or low-pressure syndromes.
- MR Spectroscopy: Helps differentiate between tumor tissue and other types of brain lesions.
6. Treatment Options: Beyond the Pill Bottle
When you see a neurosurgeon, treatment shifts from “managing symptoms” to “fixing the source.”
- Microvascular Decompression: Relieving pressure on a nerve caused by a nearby blood vessel.
- Shunt Placement: To regulate intracranial pressure in cases of hydrocephalus or IIH.
- Tumor Resection: Removing the growth that is causing pressure and pain.
- Cervical Spine Surgery: If the headache is determined to be cervicogenic, a discectomy or fusion may resolve the head pain by fixing the neck.