Minimally Invasive Spine Surgery (MISS): Advantages You Should Know
For decades, the phrase “back surgery” was often met with hesitation. Traditional spinal procedures were synonymous with large incisions, significant blood loss, and gruelling month-long recovery periods. However, the field of neurosurgery and orthopedics has undergone a seismic shift with the advent of Minimally Invasive Spine Surgery (MISS).
Today, many complex spinal conditions—from herniated discs to spinal instability—can be treated through “keyhole” incisions no larger than a postage stamp. By utilizing specialized instruments and advanced imaging, surgeons can achieve the same clinical results as traditional “open” surgery while dramatically reducing the impact on the patient’s body.
In this guide, we will explore the core advantages of minimally invasive techniques, the conditions they treat, and why MISS has become the preferred choice for both surgeons and patients.
1. What Exactly is Minimally Invasive Spine Surgery?
To appreciate the advantages of MISS, one must first understand how it differs from traditional surgery.
In traditional “open” surgery, the surgeon makes a long incision and must “strip” or pull back the muscles to reach the spinal column. This muscle retraction is often the primary cause of post-operative pain and long-term scarring.
In Minimally Invasive Spine Surgery, the surgeon uses a technique called muscle-sparing. Small incisions are made, and a series of “dilators” (small tubes) are used to gently push the muscle fibers aside rather than cutting them. The surgeon then works through a tubular retractor using an endoscope or a high-powered microscope.
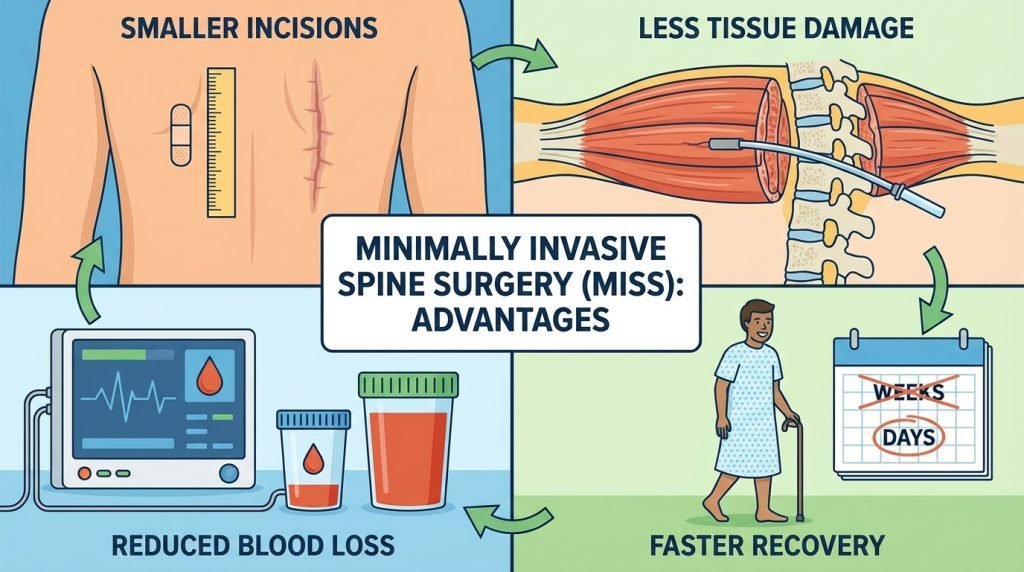
2. The Core Advantages of the Minimally Invasive Approach
The benefits of MISS extend beyond just a smaller scar. They impact every stage of the surgical journey, from the operating table to the return to work.
A. Reduced Muscle and Tissue Damage
This is arguably the most significant advantage. Because the muscles are spread apart rather than detached from the bone, the structural integrity of the back remains intact. This leads to:
- Less “surgical trauma” to the soft tissues.
- Reduced risk of permanent muscle atrophy (weakening).
- Better long-term spinal stability.
B. Minimized Post-Operative Pain
Because there is less trauma to the muscles and nerves, patients typically report significantly lower pain levels following the procedure. This leads to a decreased reliance on opioid pain medications, which is critical in modern healthcare for reducing the risk of dependency and side effects like nausea or constipation.
C. Lower Risk of Infection
Large incisions are more susceptible to bacterial contamination. Smaller incisions (often less than an inch) provide a much smaller “gateway” for infection. Clinical studies consistently show that MISS has a lower rate of surgical site infections compared to traditional open procedures.
D. Reduced Blood Loss
Traditional spine surgery can involve significant blood loss, sometimes requiring transfusions. By working through narrow corridors with precise tools, MISS minimizes damage to surrounding blood vessels. Most MISS procedures result in minimal blood loss, making the surgery safer for older adults or those with certain medical conditions.
E. Faster Recovery and Shorter Hospital Stays
Many MISS procedures are performed on an outpatient basis, meaning the patient goes home the same day. Even for more complex fusions, the hospital stay is often reduced from 5–7 days to just 1–2 days.
- Back to Work: Many sedentary workers can return to their desks within 1–2 weeks.
- Physical Activity: Patients are often encouraged to start walking the same day as surgery.
F. Better Cosmetic Results
While aesthetics are rarely the primary reason for surgery, the cosmetic benefit of MISS is undeniable. Instead of a 5-to-6-inch scar, patients are left with one or two tiny scars that often fade to near-invisibility over time.
3. Common Conditions Treated with MISS
Technological advancements have made it possible to treat a wide array of spinal issues using minimally invasive techniques:
- Herniated Discs: A Microdiscectomy is performed through a tiny incision to remove the portion of the disc pressing on a nerve.
- Spinal Stenosis: A Laminectomy can be done minimally invasively to thin out the bone and ligaments that are narrowing the spinal canal.
- Degenerative Disc Disease: Spinal Fusion (TLIF or XLIF) can be performed using percutaneous screws and rods inserted through the skin.
- Spondylolisthesis: Correcting a slipped vertebra using minimally invasive stabilization.
- Spinal Tumors: Removing certain types of tumors that are located on or near the spinal cord.
4. The Technology Behind the “Keyhole”
How does a surgeon operate on a spine they can barely see through a tiny hole? The answer lies in high-tech navigation:
- Intraoperative Fluoroscopy: Real-time X-rays that guide the surgeon to the exact vertebra.
- Surgical Robots: Robots like the Mazor or Globus system allow for sub-millimeter precision when placing spinal screws.
- Endoscopes: Tiny cameras that provide a high-definition, “close-up” view of the nerves and discs on a large monitor.
- Electromyography (EMG): Real-time nerve monitoring to ensure the surgeon does not touch or irritate vital nerve roots during the procedure.
5. Recovery Timeline: What to Expect
Recovery from MISS is categorized by “functional milestones” rather than just weeks on a calendar.
- Week 1: Focus on walking and light movement. Pain is usually managed with over-the-counter anti-inflammatories or a short course of mild pain relievers.
- Weeks 2–4: Most patients begin Physical Therapy (PT). The goal is to strengthen the core muscles that support the spine.
- Month 3: By this point, the majority of patients have returned to full activity, including sports or strenuous labor, though this depends on whether a fusion was performed.
6. Is Everyone a Candidate for MISS?
While the advantages are numerous, MISS is not for every patient. Factors that might make a traditional “open” surgery a better choice include:
- Severe Deformity: Complex scoliosis or high-grade “slipped” vertebrae may require more extensive access.
- Revision Surgery: If a patient has had previous surgery in the same area, scar tissue may make a minimally invasive approach too risky.
- Multi-Level Issues: If 5 or 6 vertebrae need to be treated simultaneously, the surgeon may opt for a traditional approach to ensure the entire area is stabilized.