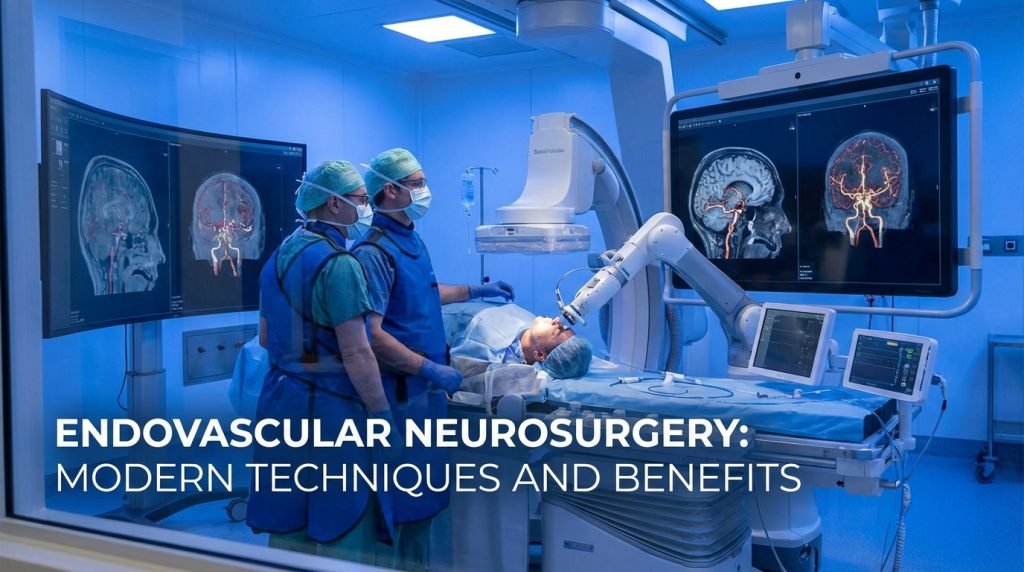
Endovascular Neurosurgery: Modern Techniques and Benefits
The landscape of neurological medicine has undergone a radical transformation over the last two decades. Traditionally, treating conditions within the brain required a craniotomy—the surgical removal of a portion of the skull to access the brain tissue. However, the advent of endovascular neurosurgery has shifted the paradigm toward minimally invasive care.
By utilizing the body’s own network of blood vessels as “highways” to reach the brain, neurosurgeons can now treat complex conditions with pinpoint precision, fewer complications, and significantly faster recovery times.
What is Endovascular Neurosurgery?
Endovascular neurosurgery (also known as interventional neuroradiology) is a subspecialty that uses catheters and radiology imaging to diagnose and treat diseases of the central nervous system. Instead of making a large incision in the skull, the surgeon makes a tiny puncture—usually in the femoral artery (groin) or the radial artery (wrist).
A thin, flexible tube called a catheter is then threaded through the arterial system under real-time X-ray guidance (fluoroscopy) until it reaches the site of the pathology in the brain or spine.
The Shift Toward Minimally Invasive Care
The primary goal of this discipline is to provide the same—or better—clinical outcomes as traditional open surgery while minimizing trauma to the patient. For many patients, this means avoiding the risks associated with general anesthesia, blood loss, and the lengthy healing process required after bone surgery.
Modern Endovascular Techniques
Technological advancements in micro-catheters, stents, and imaging software have expanded the toolkit of the modern neurosurgeon. Below are the most prevalent techniques used today.
1. Endovascular Coiling (Aneurysm Treatment)
For decades, a brain aneurysm (a bulge in a blood vessel) required a metal clip to be placed across its neck via open surgery. With endovascular coiling, the surgeon navigates a catheter into the aneurysm and releases tiny platinum coils. These coils fill the aneurysm, triggering a clot (thrombosis) that seals it off from blood flow, preventing a potentially fatal rupture.
2. Mechanical Thrombectomy (Stroke Intervention)
This is perhaps the most life-saving application of endovascular surgery. In the event of an Ischemic Stroke, where a blood clot blocks an artery in the brain, surgeons use a stent retriever or a suction device. The device “grabs” the clot and pulls it out of the body, immediately restoring blood flow.
- SEO Insight: Clinical trials have proven that mechanical thrombectomy is the “gold standard” for large vessel occlusions.
3. Flow Diversion
For large or wide-necked aneurysms that are difficult to coil, surgeons use Flow Diverters. These are specialized, high-density stents placed in the parent artery rather than the aneurysm itself. They redirect blood flow away from the aneurysm, allowing the vessel wall to heal over time.
4. Carotid Stenting
To prevent strokes caused by Carotid Artery Disease (buildup of plaque in the neck), surgeons can place a mesh stent to prop the artery open. This is often an alternative to a carotid endarterectomy (open neck surgery).
5. Embolization (AVMs and Tumors)
Arteriovenous Malformations (AVMs) are abnormal tangles of blood vessels. Using “liquid embolic agents” (a type of medical glue), surgeons can plug these dangerous vessels. This technique is also used to cut off the blood supply to brain tumors before a surgical removal, making the final operation much safer.
The Major Benefits of Endovascular Procedures
The transition from “open” to “endovascular” offers several measurable benefits for patients and healthcare systems alike.
1. Reduced Recovery Time
In an open craniotomy, patients may spend a week in the hospital and months recovering at home. With endovascular techniques, most patients are discharged within 24 to 48 hours and can return to light activities within a week.
2. Minimal Physical Trauma
Because the entry point is a needle puncture rather than a surgical incision, there is no large scar and significantly less post-operative pain. This also reduces the risk of surgical site infections, which is a major concern in traditional neurosurgery.
3. Access to “Inoperable” Areas
Some aneurysms or malformations are located deep within the brain stem or in areas where open surgery would cause catastrophic collateral damage. Endovascular tools can reach these areas safely through the internal vasculature.
4. Use of Conscious Sedation
Many endovascular procedures can be performed while the patient is under conscious sedation (awake but relaxed) rather than general anesthesia. This is particularly beneficial for elderly patients or those with heart conditions who may not tolerate being “put under” for long periods.
Conditions Treated with Endovascular Neurosurgery
As the field evolves, the list of treatable conditions continues to grow:
- Brain Aneurysms: Both ruptured and unruptured.
- Acute Ischemic Stroke: Emergency clot removal.
- Arteriovenous Malformations (AVM): Tangles of vessels.
- Carotid Stenosis: Narrowing of the neck arteries.
- Epistaxis: Severe, life-threatening nosebleeds.
- Intracranial Atherosclerosis: Narrowing of arteries inside the brain.
- Venous Sinus Stenosis: Often treated to relieve Idiopathic Intracranial Hypertension (IIH).
The Future: Robotics and Artificial Intelligence
The next frontier for endovascular neurosurgery is the integration of robotic-assisted platforms. These systems allow for even greater precision in catheter movement, potentially allowing surgeons to perform procedures remotely. Furthermore, AI-driven imaging helps surgeons predict which patients will benefit most from thrombectomy by analyzing brain tissue viability in seconds.