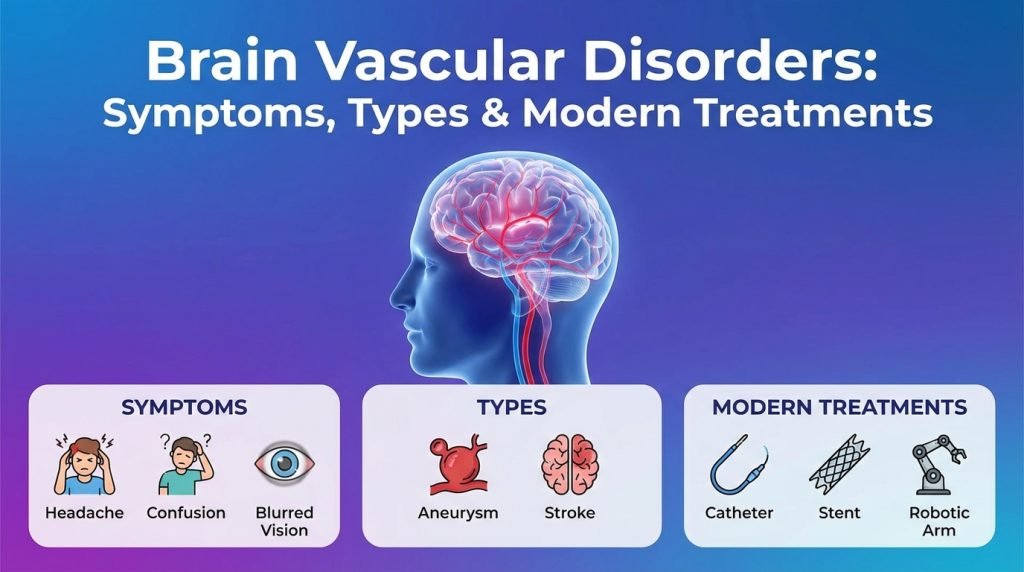
Brain Vascular Disorders: Symptoms, Types & Modern Treatments
The human brain is an incredibly demanding organ, consuming roughly 20% of the body’s oxygen and nutrients despite making up only 2% of its weight. This constant demand is met by a complex network of blood vessels. When something goes wrong with this “plumbing”—a condition known as a brain vascular disorder or cerebrovascular disease—the results can be life-altering.
Brain vascular disorders encompass a variety of conditions that affect the blood vessels and blood supply to the brain. From sudden events like strokes to “silent” conditions like aneurysms, understanding the symptoms and the latest medical interventions is critical for prevention and recovery.
1. Common Types of Brain Vascular Disorders
To understand the treatment, we must first categorize the most common types of vascular issues that occur within the cranium.
Brain Aneurysms
A brain aneurysm is a weak or thin spot on an artery wall that balloons out and fills with blood. The primary danger is that the aneurysm may leak or rupture, causing a life-threatening subarachnoid hemorrhage.
Arteriovenous Malformations (AVM)
An AVM is an abnormal “tangle” of blood vessels connecting arteries and veins in the brain. This tangle disrupts normal blood flow and can lead to bleeding or seizures because the vessels are often weaker and prone to rupture.
Carotid Artery Disease
The carotid arteries are the major blood vessels in the neck that supply the brain. In carotid artery disease, these vessels become narrowed or blocked by fatty deposits (plaque), significantly increasing the risk of an ischemic stroke.
Cavernous Malformations
Also known as cavernomas, these are clusters of abnormal, “mulberry-shaped” capillaries in the brain or spinal cord. They leak blood slowly, which can cause neurological symptoms or seizures over time.
Stroke (Ischemic and Hemorrhagic)
- Ischemic Stroke: A blockage (clot) prevents blood from reaching a part of the brain.
- Hemorrhagic Stroke: A blood vessel ruptures, causing bleeding into the brain tissue.
2. Recognizing the Symptoms: The Warning Signs
Because the brain controls every function of the body, the symptoms of a vascular disorder depend entirely on which part of the brain is affected.
The “Thunderclap” Headache
Often associated with a ruptured aneurysm, a thunderclap headache is a sudden, excruciating pain that reaches maximum intensity within 60 seconds. Patients often describe it as the “worst headache of their life.”
The FAST Acronym for Stroke
If you suspect a vascular event, use the FAST check:
- F (Face): Does one side of the face droop when smiling?
- A (Arms): Does one arm drift downward when raised?
- S (Speech): Is the speech slurred or strange?
- T (Time): If these signs are present, call emergency services immediately.
Other Neurological Deficits
- Vision Changes: Sudden loss of vision in one eye or double vision.
- Pulsatile Tinnitus: A rhythmic thumping or “whooshing” sound in the ear that matches your heartbeat (often a sign of a dural arteriovenous fistula).
- Seizures: New-onset seizures in an adult can be a sign of an AVM or cavernoma.
- Cognitive Decline: Difficulties with memory or executive function caused by “small vessel disease” or multiple mini-strokes (TIAs).
3. How Brain Vascular Disorders are Diagnosed
Modern neuro-imaging has revolutionized the way we detect vascular issues, often finding them before they rupture.
- CT Angiography (CTA): A fast, non-invasive scan that uses a special dye to visualize the blood flow in the brain’s arteries.
- Magnetic Resonance Angiography (MRA): Similar to a CTA but uses magnetic fields. It is excellent for finding unruptured aneurysms without using radiation.
- Digital Subtraction Angiography (DSA): The “gold standard” for vascular diagnosis. A catheter is threaded from the groin to the brain, and dye is injected. This provides the most detailed “map” of the brain’s vessels.
- Carotid Ultrasound: A simple, non-invasive test used to check for blockages in the neck arteries.
4. Modern Treatment Options: The Shift to Minimally Invasive Care
In the past, most brain vascular issues required “open” surgery. Today, endovascular neurosurgery allows many conditions to be treated from inside the blood vessel.
Endovascular Coiling and Stenting
For aneurysms, a surgeon threads a catheter to the site and fills the aneurysm with tiny platinum coils. These coils trigger a clot, effectively “sealing off” the aneurysm from the rest of the blood flow. A stent may be used to keep the artery open.
Flow Diverters
One of the most modern advancements is the Flow Diverter (Pipeline). This is a specialized stent placed in the main artery past the aneurysm. It redirects blood flow away from the aneurysm, causing it to shrink and heal over time without the need for coils.
Surgical Clipping
In some cases, traditional surgery is still the safest option. A neurosurgeon performs a craniotomy and places a tiny metal clip across the neck of the aneurysm to stop it from bleeding.
Stereotactic Radiosurgery (Gamma Knife)
For deep-seated AVMs that are too risky to reach with traditional surgery, Gamma Knife uses highly focused radiation to shrink and eventually close the abnormal blood vessels over a period of 1 to 3 years.
Carotid Endarterectomy & Stenting
To treat carotid artery disease, surgeons can either surgically remove the plaque (Endarterectomy) or use a balloon to stretch the artery and place a metal stent to keep it open.
5. Risk Factors and Prevention
While some vascular disorders are congenital (present from birth), many are related to lifestyle and can be managed.
- Hypertension (High Blood Pressure): The leading cause of vascular rupture. Maintaining a blood pressure below 120/80 is vital.
- Smoking: Chemicals in tobacco weaken the walls of the arteries, making aneurysms more likely to form and burst.
- Cholesterol Management: High LDL levels lead to plaque buildup in the carotid arteries.
- Genetic Predisposition: If two or more immediate family members have had a brain aneurysm, screening is highly recommended.
6. Recovery and Long-Term Outlook
Recovery from a brain vascular event depends on the speed of treatment.
- Endovascular Recovery: Patients often go home within 24–48 hours and can return to light activity within a week.
- Hemorrhage Recovery: If a rupture has occurred, recovery involves intensive rehabilitation (physical, occupational, and speech therapy) to help the brain reroute signals.