Brain Hemorrhage: Early Warning Signs & Emergency Care
A brain hemorrhage—commonly referred to as a “brain bleed”—is a life-threatening medical emergency. It is a type of stroke caused by an artery in the brain bursting, which leads to localized bleeding in the surrounding tissues. This bleeding kills brain cells by depriving them of oxygen and creating life-threatening pressure within the skull.
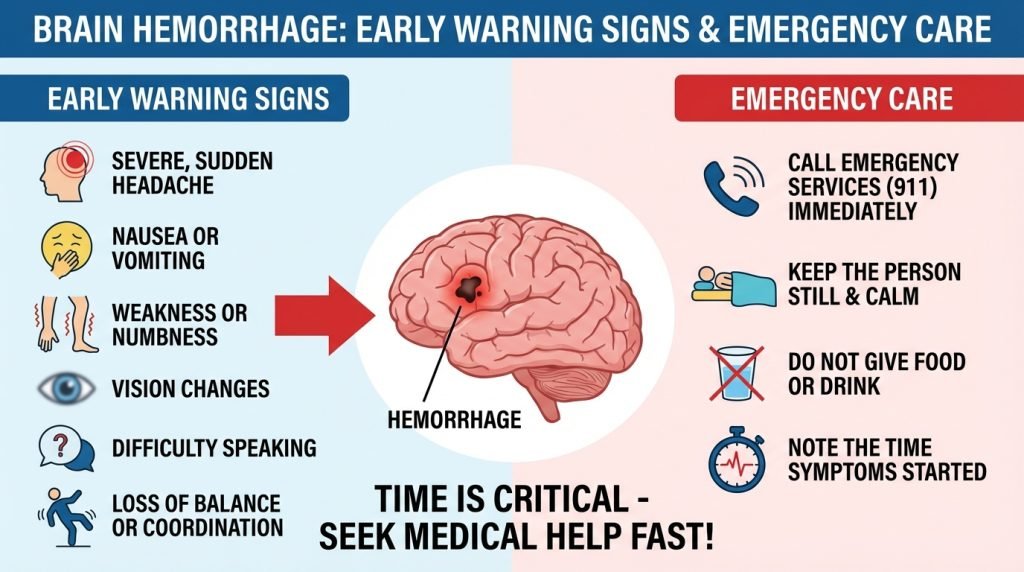
When it comes to a brain hemorrhage, every second counts. Neurologists often use the phrase “Time is Brain,” meaning the faster a patient receives treatment, the higher their chances of survival and recovery. This guide outlines the early warning signs, different types of hemorrhages, and the critical steps for emergency intervention.
1. What is a Brain Hemorrhage?
A brain hemorrhage is technically known as an intracranial hemorrhage. When a blood vessel ruptures, the blood pools. This collection of blood, known as a hematoma, increases pressure on the brain (intracranial pressure) and reduces vital blood flow to certain regions.
The Different Types of Brain Bleeds
Hemorrhages are classified by exactly where the bleeding occurs:
- Intracerebral Hemorrhage: Bleeding occurs inside the brain tissue itself. This is the most common type of hemorrhagic stroke.
- Subarachnoid Hemorrhage: Bleeding occurs between the brain and the thin tissues that cover it. This is often caused by a ruptured aneurysm.
- Epidural and Subdural Hematomas: These usually occur due to head injuries. Bleeding happens between the skull and the brain’s protective covering (dura) or just below the dura.
2. Early Warning Signs: Identifying a Brain Bleed
The symptoms of a brain hemorrhage can come on very suddenly. While they can mimic the signs of a typical ischemic stroke, certain “red flags” are more common with bleeding.
The “Thunderclap” Headache
The most iconic sign of a subarachnoid hemorrhage is a “Thunderclap Headache.” Patients often describe this as the “worst headache of my life.” It reaches peak intensity within seconds or minutes and feels like a sudden, blinding blow to the head.
Sudden Neurological Deficits
If the bleed is occurring in a specific part of the brain, you may notice:
- One-Sided Weakness: Sudden numbness or tingling in the face, arm, or leg, usually on just one side of the body.
- Vision Changes: Sudden loss of vision, blurred vision, or double vision.
- Speech Difficulties: Difficulty speaking (slurred speech) or difficulty understanding what others are saying.
- Loss of Coordination: Sudden dizziness, loss of balance, or inability to walk.
Other Physical Signs
- Nausea and Projectile Vomiting: Intense vomiting that occurs suddenly and without warning is a common sign of rising intracranial pressure.
- Seizures: A sudden seizure in someone who does not have epilepsy is a major red flag.
- Confusion or Lethargy: A rapid drop in alertness or a sudden “fading” of consciousness.
3. Causes and Risk Factors
Understanding the causes of a brain hemorrhage can help in prevention and early detection.
- High Blood Pressure (Hypertension): This is the #1 cause of brain hemorrhages. Over time, high pressure weakens the walls of the arteries until they burst.
- Head Trauma: Falls, car accidents, or sports injuries are the leading cause of brain bleeds in younger populations.
- Aneurysm: A weak, bulging spot on an artery wall that eventually thins and ruptures.
- Amyloid Angiopathy: An abnormality of the blood vessel walls that sometimes occurs with aging and high blood pressure.
- Blood Thinners: Medications like warfarin or aspirin can increase the risk of bleeding or make a minor bleed much worse.
- Blood Vessel Abnormalities: Conditions like Arteriovenous Malformations (AVMs) are weak connections between arteries and veins present from birth.
4. Emergency Care: What to Do Immediately
If you suspect someone is experiencing a brain hemorrhage, do not wait to see if the symptoms pass.
Step 1: Call Emergency Services
Dial 911 or your local emergency number immediately. Inform the operator that you suspect a stroke or brain hemorrhage. This ensures the hospital is prepared with neurosurgical staff upon your arrival.
Step 2: Use the FAST Check
While waiting for the ambulance, use the FAST acronym to assess the person:
- F (Face): Ask them to smile. Does one side of the face droop?
- A (Arms): Ask them to raise both arms. Does one arm drift downward?
- S (Speech): Ask them to repeat a simple phrase. Is their speech slurred or strange?
- T (Time): If you see any of these signs, it is time to call 911.
Step 3: Critical Precautions
- Do not give the person medication: Do not give them aspirin. If the stroke is a hemorrhage, aspirin will thin the blood and make the bleeding worse.
- Do not give food or water: A brain hemorrhage can affect the ability to swallow, leading to choking.
- Keep them still: Lay the person on their side with their head slightly elevated to help reduce pressure and prevent choking if they vomit.
5. Hospital Diagnosis and Treatment
Once at the hospital, the medical team will work rapidly to confirm the bleed.
Diagnosis
- CT Scan: This is the fastest way to detect fresh blood in the brain. It is the primary tool used in emergency rooms.
- MRI: Provides a more detailed look at the brain tissue to find the underlying cause of the bleed.
- Angiogram: A catheter is threaded through the arteries to look for aneurysms or AVMs.
Treatment
Treatment focuses on stopping the bleeding, reducing pressure, and preventing further damage:
- Medications: Doctors use drugs to aggressively lower blood pressure and counteract any blood thinners the patient may be taking.
- Surgery: If the bleed is large, a neurosurgeon may perform a craniotomy to remove the pooled blood (hematoma) and relieve pressure on the brain.
- Aneurysm Clipping/Coiling: If an aneurysm caused the bleed, surgeons will use a tiny metal clip or a wire coil to “plug” the leak.
6. Recovery and Long-Term Outlook
Recovery from a brain hemorrhage depends on the size of the bleed and how quickly it was treated. Some patients make a full recovery, while others may face long-term challenges.
- Rehabilitation: Most survivors require physical, occupational, or speech therapy to relearn skills and regain strength.
- Preventing a Second Bleed: This involves strict management of blood pressure, quitting smoking, and regular follow-ups with a neurologist.