Endoscopic Brain Surgery: Benefits, Techniques, and Recovery
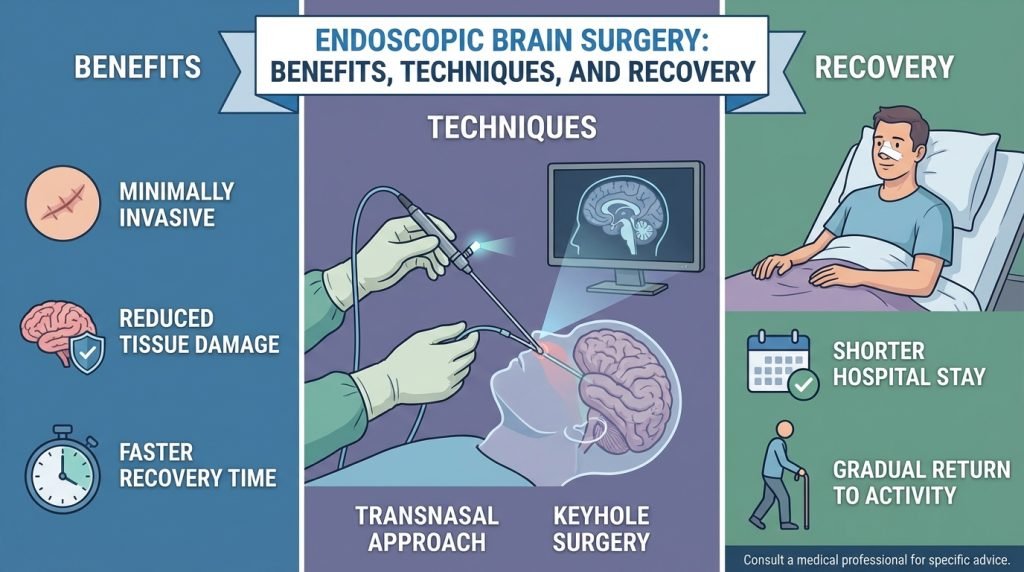
The field of neurosurgery has undergone a silent revolution. Gone are the days when every brain-related procedure required a large, invasive “open” craniotomy. Today, endoscopic brain surgery allows neurosurgeons to treat complex conditions through tiny incisions or even natural openings like the nostrils.
For patients and families, this shift means less trauma, fewer complications, and a significantly faster return to daily life. In this guide, we explore the mechanics of endoscopic neurosurgery, its primary benefits, and what to expect during the recovery phase.
What is Endoscopic Brain Surgery?
Endoscopic brain surgery is a minimally invasive technique where a neurosurgeon uses a thin, flexible tube called an endoscope. This device is equipped with a high-definition camera and a powerful light source, transmitting real-time images of the brain to a monitor in the operating room.
Unlike traditional surgery, which requires a large opening in the skull to provide the surgeon with a “line of sight,” the endoscope can navigate around the delicate structures of the brain. The surgeon reaches the target area through:
- The Endonasal Approach: Entering through the nose (commonly used for pituitary tumors).
- Keyhole Surgery: Entering through a small “burr hole” in the skull, often no larger than a dime.
Key Conditions Treated with Endoscopic Techniques
Endoscopy is not suitable for every brain condition, but it has become the “gold standard” for several specific diagnoses:
- Pituitary Tumors: Located at the base of the brain, these are most commonly reached through the nasal passages (Endoscopic Endonasal Approach).
- Hydrocephalus: A condition where excess fluid builds up in the brain. Surgeons use an endoscope to perform a Third Ventriculostomy, creating a bypass for the fluid.
- Colloid Cysts: Small fluid-filled sacs in the centre of the brain that can be safely drained or removed via a keyhole incision.
- Skull Base Tumors: Meningiomas or chordomas located in hard-to-reach areas at the bottom of the cranial vault.
- Cerebrospinal Fluid (CSF) Leaks: Repairing the “leaks” that cause brain fluid to exit through the nose or ears.
The Major Benefits of Endoscopic Brain Surgery
When compared to traditional “open” surgery, the benefits of the endoscopic approach are profound for both the clinical outcome and the patient’s psychological well-being.
1. Minimized Trauma to Brain Tissue
In a traditional craniotomy, the surgeon often has to retract (move aside) healthy brain tissue to reach a tumor. This can cause temporary or permanent neurological deficits. An endoscope, however, “threads” through the natural corridors of the brain, minimizing brain retraction and preserving healthy tissue.
2. Superior Visualization
The endoscope provides a “close-up” view that even a surgical microscope cannot match. It allows the surgeon to see around corners and behind structures, ensuring that the entire tumor is removed while protecting vital nerves and blood vessels.
3. Reduced Risk of Infection and Scarring
Smaller incisions mean a smaller gateway for bacteria. Additionally, for patients undergoing the endonasal approach, there are no visible external scars, as the entire procedure is performed internally through the nostrils.
4. Shorter Hospital Stays
While a traditional brain surgery might require a week-long hospital stay, many endoscopic patients are discharged within 2 to 3 days, provided there are no complications.
The Recovery Journey: What to Expect
Recovery from brain surgery is a gradual process. While endoscopy is “minimally invasive” on the outside, significant work has still been done on the inside.
Phase 1: The Hospital Stay (Days 1–3)
Immediately after surgery, you will be monitored in the Neurological Intensive Care Unit (ICU) or a specialized step-down unit.
- Monitoring for CSF Leaks: If the surgery was done through the nose, doctors will watch closely for clear fluid dripping from the nose, which could indicate a leak.
- Pain Management: Patients usually report less pain than open surgery, but “pressure headaches” are common.
- Nasal Packing: If an endonasal approach was used, you may have packing in your nose, making it feel like a severe head cold.
Phase 2: The First Two Weeks at Home
Once discharged, the focus shifts to rest and wound healing.
- Activity Restrictions: No heavy lifting (usually nothing over 5–10 lbs), no strenuous exercise, and no bending over with your head below your waist.
- Nasal Care: Patients are often prescribed saline nasal sprays or rinses to keep the nasal passages clean and prevent crusting. Do not blow your nose until cleared by your surgeon, as this can create pressure that disrupts the healing site.
- Fatigue: It is normal to feel very tired. Your brain is using significant energy to heal from the surgical intervention.
Phase 3: Returning to Normalcy (Weeks 4–8)
Most patients can return to light work and driving within 4 to 6 weeks.
- Follow-up Imaging: You will likely have an MRI 6 to 12 weeks after surgery to ensure the tumor has not recurred and the surgical site is stable.
- Long-term Outlook: For many, the symptoms that led to surgery (vision loss, hormonal imbalances, or headaches) begin to improve significantly during this window.
Potential Risks and Complications
While the risks are lower than open surgery, they are not zero. Potential complications include:
- CSF Leak: Fluid leaking from the brain through the nose.
- Meningitis: An infection of the protective membranes covering the brain.
- Hormonal Changes: Particularly common after pituitary surgery, requiring temporary or permanent hormone replacement therapy.